Understanding Pericardial Effusion
Pericardial effusion is the buildup of extra fluid in the sac around the heart. If too much fluid builds up, it can put pressure on the heart. This can prevent it from pumping normally.
How to say it
Pair-ih-CAR-dee-ull
Eff-YOO-zhun
How pericardial effusion happens
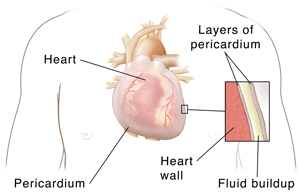
A fibrous sac surrounds your heart. The sac is called the pericardium. It’s made of 2 thin layers with a small amount of fluid between them. The fluid helps cushion the 2 layers as they rub against each other when the heart beats. In some cases, extra fluid can build up between these layers. This is called pericardial effusion.
Pericardial effusion can sometimes happens quickly. This is known as acute pericardial effusion. Other times, the fluid builds up slowly. This is known as subacute pericardial effusion. Pericardial effusion that occurs more than once over time is called chronic pericardial effusion.
A little fluid won’t cause much of a problem, but too much fluid can put pressure on the heart. This makes it hard for the heart to pump normally. This is called cardiac tamponade. It often needs emergency treatment. Because of the extra pressure, less blood can enter the heart from the body. Less oxygen-rich blood will go out to the body. But not all cases of pericardial effusion cause cardiac tamponade.
What causes pericardial effusion?
Sometimes, the cause of fluid buildup is not known. But a number of conditions can cause extra fluid in the pericardium. These include:
-
Infection of the pericardium caused by viruses, bacteria, fungi, or parasites.
-
Cancer. Lung cancer is the most common cause of malignant pericardial effusion.
-
Inflammation of the pericardium because of a heart attack.
-
Trauma from blunt, penetrating injuries, including injuries from medical procedures on the heart.
-
Auto-immune disorders, including systemic lupus erythematosus, rheumatoid arthritis, and Sjögren's syndrome.
-
Reactions to certain medicines.
-
Radiation.
-
Metabolic causes, such as kidney failure with uremia (a buildup of waste products in the blood that are normally removed by the kidney).
-
Heart failure.
-
Other health conditions. These include cirrhosis of the liver, hypothyroidism leading to myxedema, or ovarian hyperstimulation syndrome.
What are the symptoms of pericardial effusion?
If you have mild pericardial effusion, you may not have any symptoms. You might be more likely to have symptoms from whatever is causing the pericardial effusion. For example, you might have a fever if you have an infection of the pericardium.
If the effusion is more severe, you may have symptoms, such as:
-
Chest pain or discomfort. It improves when you sit upright, and it gets worse when you lie flat.
-
Shortness of breath.
-
Fast breathing.
-
Increased heart rate and palpitations.
-
Enlargement of the veins of the neck.
-
Fainting.
-
Swelling in the arms and legs.
-
Pain in the right upper abdomen.
-
Nausea.
If the effusion is very severe, it can also lead to very low blood pressure. This can cause symptoms of shock, like cool arms and legs, pale skin, and less urine. Shock is a medical emergency.
How is pericardial effusion diagnosed?
Your health care provider will ask about your health history and your symptoms. They will also give you a physical exam. For symptoms of shock, it’s important to find the cause quickly.
You may also have tests, such as:
-
Echocardiogram. It's most commonly used for diagnosis that looks at fluid around the heart and the heart’s motion.
-
Electrocardiogram to look at the heart’s electrical rhythm.
-
Chest X-ray to see the heart anatomy.
-
CT scan or MRI scan to see more detail of the heart anatomy. They also help in looking at the entire chest to find anything in the lungs or next to the lungs that isn't normal.
You may also have tests to find the cause of the pericardial effusion, such as:
-
Blood tests to look for infection, immune system problems, or metabolic problems.
-
Tests of the fluid removed from around the heart to check for cancer or infection.